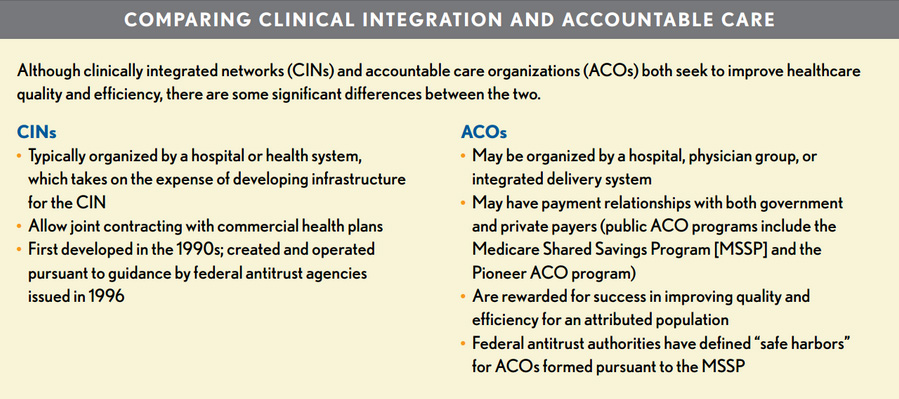
Comparing Clinical Integration & ACO‘s
These arrangements are both designed to improve the efficiency and quality of health care. Although they share similar goals, there are important distinctions between the two. CINs are typically organized by a hospital or health system and bring both independent and employed physicians together into an integrated network designed to improve the quality and efficiency of healthcare services. A 1996 statement from the federal antitrust enforcement agencies— the Federal Trade Commission (FTC) and Department of Justice (DOJ)—allowed parties to a CIN to jointly contract with payers, provided that:
- The CIN features clinical integration involving authentic initiatives that require the active participation of all network participants in an ongoing program to evaluate and modify practice patterns
- The program is designed to achieve likely improvements in healthcare quality and efficiency
- Joint contracting with a health plan is reasonably necessary to achieve the efficiencies of the clinical integration program. Contracts with the CIN will typically involve some form of value-based incentive (e.g., pay for performance, shared savings) that rewards the network for success in achieving its efficiency goals.
CINs first appeared in the 1990s and thus predate ACOs by about two decades. Clinical integration is a necessity for an ACO, but a CIN does not have to become an ACO. There are both “public” and “private” forms of ACOs. Public ACOs include those formed pursuant to provisions in the Affordable Care Act (ACA) that authorized the Medicare Shared Savings Program (MSSP) and the Center for Medicare & Medicaid Innovation’s Pioneer ACO Program.
On the private side, many commercial health plans are working with physicians, hospitals, and other providers to form ACOs. There is significant overlap between the two; an ACO that was formed to participate in the MSSP may also seek a commercial ACO contract with a health plan, for example.
A key distinction between ACOs and CINs is that ACOs are closer to a population management model in that they are designed to improve the quality and reduce the cost of care for an attributed population. They are typically rewarded with a share of the savings if they can reduce the cost of care for the attributed population below a historical benchmark while maintaining or improving the quality of outcomes for that population. Depending on the payment model, they might also be asked to share in the loss if costs of care exceed the historical benchmark.
To promote the formation of ACOs and the required collaboration among providers, the FTC and DOJ have created “safe harbors” from antitrust scrutiny for ACOs that fall below defined market share percentage thresholds* The ACA authorized waivers of fraud and abuse laws to permit funding of an ACO’s development (e.g., investment in a shared IT platform), distribution of shared savings among ACO participants, and the provision of nonmonetary preventive items or services (e.g., heart-rate monitors) to Medicare beneficiaries. With respect to independent physician practices, both CINs and ACOs give hospitals and health systems a means of tightening their alignment with these practices while avoiding some of the potential financial costs of full employment. As the organizer of a CIN, the hospital or health system will still face significant costs to develop the necessary infrastructure for the network, including a common IT platform and care managers. Physicians in the market also have to be ready to integrate, which will typically include acceptance of quality metrics and care protocols designed to improve quality and efficiency.
*An accountable care organization (ACO) falls within a “safe harbor” if independent ACO participants that provide the same service (a “common service”) have a combined share of 30 percent or less of each common service in each participant’s primary service area, wherever two or more of the ACO participants provide that service to patients from that primary service area. The statement by the Federal Trade Commission and Department of Justice also offers guidance for ACOs outside the safe harbor, including a summary of conduct to avoid and a process for expedited antitrust review of a proposed ACO (“Statement of Antitrust Enforcement Policy Regarding Accountable Care Organizations Participating in the Medicare Shared Savings Program,” Federal Register, Oct. 28, 2011.

